 What is the treatment for acute lymphoblastic leukemia in children? At this time, your child, or someone you love or know, have had the diagnosis of childhood leukemia, You are probably wondering what comes next? The treatment for ALL typically involves a combination of therapies designed to achieve remission, prevent the cancer from coming back, and manage any side effects. The exact treatment plan can vary depending on factors such as the patient’s age, overall health, specific subtype of ALL, and the extent of the disease.
What is the treatment for acute lymphoblastic leukemia in children? At this time, your child, or someone you love or know, have had the diagnosis of childhood leukemia, You are probably wondering what comes next? The treatment for ALL typically involves a combination of therapies designed to achieve remission, prevent the cancer from coming back, and manage any side effects. The exact treatment plan can vary depending on factors such as the patient’s age, overall health, specific subtype of ALL, and the extent of the disease.
My daughter’s own treatment, 30 years ago at the time of writing this article, almost 3 years and then we waited for 5 more years of having regular blood tests before they declared her to be in Remission and unlikely to relapse. You would have to check yourselves what the current time frame is due to the changing nature of treatment protocols, but knowing that you could be in for the long haul might help you be able to prepare yourselves a little better. Don’t let the medical professionals downplay the side effects, both immediate and long-term, because there are many and it’s better to know what you may be facing now, and down the track, and learn how to deal with things when they crop up or, or get the help you need before things get out of control. I will say more on this in other articles, for now we will just be discussing the treatment protocol in terms of the 3 phases. A second article (insert link) will delve into more of the treatment, including surgery. Over the two articles I will be naming some of the drugs used in the chemotherapy treatment but won’t go into the side effects of them at this stage. If you wish to know more on this, you can look them up individually or wait for my article on these to be written.
Treatment Overview for Childhood Acute Lymphoblastic Leukemia (ALL)
Knowledge in advance can go a long way to helping you get through the challenges you will be facing. Leukemia and the treatment for it, can heavily impact yours and their entire lives. Here are just a few impacts that we will discuss throughout the articles on my website; financial, social, brain functioning, psychological, isolation, marriage strain, lack of support, friendships, ability to go places, ADD/ADHD, Developmental/Complex PTSD, hospitalisation for extended periods of time, job retainment, schoolwork, susceptibility to other life threatening illnesses and even the roof over your head. Here is a brief overview of the typical treatment components for ALL to help you understand what areas of the body are targeted, how, the drugs are administered, Intravenous, intramuscular, orally and into spinal fluid, and what to expect in this regard, and I’ve included a few other things to be aware of as well.
Phase I: Induction Therapy:
This is the initial phase of treatment which aims to induce patient remission by killing the majority of leukemia cells in the  bone marrow. It is usually one of the shorter periods of time, a matter of 4 weeks of very intensive treatment and this time you would expect to be in hospital.
bone marrow. It is usually one of the shorter periods of time, a matter of 4 weeks of very intensive treatment and this time you would expect to be in hospital.
Some common drugs used during induction therapy include Prednisone, Vincristine, Daunorubicin (known as the Red Devil), and Asparaginase. These drugs are often administered intravenously or orally.
It was during and after this treatment phase that my daughter began to lose her hair which fell out over about a period of 2 to 4 weeks. Some children put on a lot of weight in their faces due to the Prednisone, which is a steroid drug. I believe it was mostly fluid build up that caused patients to gain the weight. My daughter seemed to avoid this side effect, but many other children were affected.
Treatment Came With It’s Fair Share Of Other Problems
The treatment alone was bad enough, however there were other problems and side effects that surfaced with it that might not have been discussed with your health care professionals or thought about until they occurred. While everyone has their own personal experiences which may vastly differ from other people, some may be more universal and it’s better to be forewarned so you can prepare.
Abandon my Daughter? No Way!
In these early days of diagnosis, they tried to make me leave my very young child in the hospital alone at night time while they had me stay at a unit about a 15 minute walk away from the hospital. At first I did this because it sounded like I had no choice, but she was just so young I couldn’t bear to leave her all alone and possibly feeling abandoned, so I made it clear to them that I didn’t want to do this anymore. The hospital arranged a fold up stretcher bed for me to sleep on and I stayed with her the entire time, only folding up the bed during the day and slotting it in behind her bed out of the way. I fear the damage may have already been done by then but that didn’t rear it’s head until sometime later. If you are like me, you may want to push them to do the same for you. They would only permit one person to stay with the child so you may need to take turns if you have a partner, or have the one dedicated parent stay.
Phase II: Consolidation (Intensification) Therapy:
After achieving remission, Consolidation Therapy is used to further eliminate any remaining leukemia cells and reduce the risk of relapse. It often involves additional courses of chemotherapy over multiple cycles of therapy which may last 6 to 9 months. It is still an intensive treatment phase and your child may require some hospitalisation, blood and platelets transfusions due 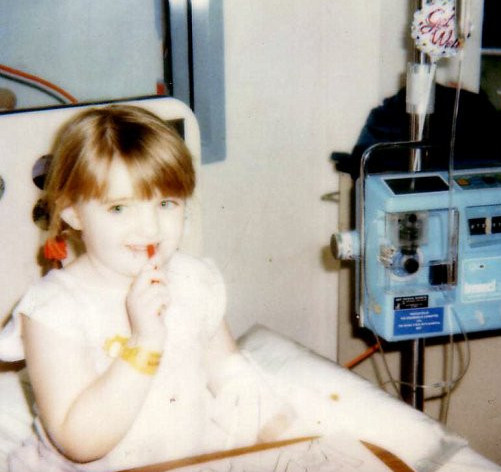 to the aggressive nature of the treatment and the need for intensive support and monitoring of your child. Ara-C, 6-Mercaptopurine and Methotrexate are among the chemotherapy drugs used in this phase.
to the aggressive nature of the treatment and the need for intensive support and monitoring of your child. Ara-C, 6-Mercaptopurine and Methotrexate are among the chemotherapy drugs used in this phase.
Can I Expect Long Stays In Hospital?
The answer is a resounding “Yes”. Just to give you an idea of what we went through, our first 3 months of treatment were spent in hospital nearly the entire time, and many more times were spent in hospital if my daughter got a high temperature, we could expect to stay in the hospital for up to 10 days while they did tests to determine what infection she had, if she had an infection at all, or whether it was a response to the treatment. We also found that during this time, they overdid her treatment in terms of the chemotherapy acting too rapidly on her cells and they had to keep stopping treatment because she was losing blood and other cells too fast and they needed to build back up again, hence the need for blood and platelets transfusions during this phase. I am writing some articles on ideas of what to bring to the hospital if you find yourself, which you will, driving to the hospital in the middle of the night.
Will Treatment be Hit and Miss?
Quite possibly! At one stage she got so bad that they thought she had relapsed, which was just one more added stress at the time for me, more tests for her and the waiting game to find out if the news was good or bad. Thankfully she hadn’t relapsed and it was determined that the treatment dosages were too high for her little body to recover and replenish in time for the next bout of chemotherapy, so they had to reduce the dosages by trial and error until they got it right. As a parent, you can do nothing much but sit back chewing your fingernails and watch them do what they need to do and hope for the best and that no errors will be made and that the treatment will save your child. It was horrible going through this as a parent, let alone how it must’ve been for my daughter. My suggestion to you is to keep an eye on your child. A good way to determine if there are any problems during the longer phases where there are less blood tests, is to check the palms of your child’s hands and if the lines are white, then it’s quite likely that they have low red blood cells and may need a transfusion. If they are bruising easily or their skin is showing petechiae, little red dots that look like broken capillaries, it can be a sign of low platelets. Usually they will send you for a blood test if these things occur and they will decide from there if transfusions are needed, hospital stays or just to simple stop treatment for a little while. It’s all a bit of a balancing act as you will find.

Phase III: Maintenance Therapy:
Following consolidation therapy, patients typically enter a maintenance phase, which involves lower doses of chemotherapy drugs over an extended period, often several years. This phase helps to keep any remaining leukemia cells in check and prevent relapse. Treatment is usually between 18 months to 2 years and this phase of the treatment is what takes up most of the time overall. You may be required to take oral medication daily or weekly, have some intravenous chemotherapy weekly and possibly intramuscular chemotherapy as well.
Is it Better to Go to Your Local Hospital for Convenience?
There are Definitely Pros and Cons to it! We were able to have most of this phase of the treatment at our local hospital’s oncology ward instead of having to drive an hour and a half away for the treatment, which helped us feel like there was a modicum of normality to our lives. This was a blessing for the most part, but also being unfamiliar with my daughter and what the usual protocols were with her, there were often problems coming up with having “strangers” treat her. My mother used to come with me for as a support for both of us. There were two things we didn’t look forward to in this phase. The delivery method for the treatment and the impact it might have on my child and whether or not the staff would use the same equipment my daughter was used to.
“It’s Too Big!”
You need to listen to the kids, they know! My daughter still hated having her porta-cath needled and was very attuned to exactly what sized needle her normal hospital  used. She kicked and screamed so much one day shouting “it’s too big, it’s too big” that we had to try and work out what was wrong with her. It turned out that they were trying to re-needle it with one that was more than twice the size of the one normally used by the main hospital and she knew exactly what size it should have been. Thankfully the nurses listened to her protests and called our primary hospital to find out what sized needle they normally used and they fixed the problem.
used. She kicked and screamed so much one day shouting “it’s too big, it’s too big” that we had to try and work out what was wrong with her. It turned out that they were trying to re-needle it with one that was more than twice the size of the one normally used by the main hospital and she knew exactly what size it should have been. Thankfully the nurses listened to her protests and called our primary hospital to find out what sized needle they normally used and they fixed the problem.
Oh My God that Hurts!
Yes it does, a LOT! The other thing was that some of the chemo was delivered intramuscularly, and it really HURT my daughter. I would have to sit my daughter on my lap facing me with her arms crossed in front of her to restrain her yet be giving her a loving hug, while my Mum used to have to stand behind me and hold my daughters legs down so she couldn’t pull away while they administered the drug via needle right into her leg. It was one of the things my Mum hated having to do, but she came with me to help anyway because she knew I would have to do it alone otherwise. I hated it too by the way. These things affect the parent and in this case grandparents too and leave you feeling like such an awful parent. It was one of my greatest fears, that my daughter would hate me for allowing these things to happen to her and sadly, it did have an effect like this down the track.
Will Mistakes Be Made?
I hope not, but there are no guarantees! Another time there was a mishap with the dosages of her medications provided. We had to stay in that same local hospital one time when she had a temperature and when we arrived, they told me they couldn’t use the medications that I provided which I had bought and paid for at her primary hospital, and had to draw up their own through their pharmacy. However 3 days later when they told us we could go home, they gave me all of the unused medications for me to take home with me and continue to use them at home. Upon checking them, I realised that they had drawn up the wrong amounts of 2 of the medications. One was 4 times the amount it was supposed to be, and the other was half the amount, and they had been giving her these medications instead of the correct ones that I tried to supply them with. Luckily there was no lasting damage that time, that we know of anyway. Needless to say, we never went back to that hospital if it meant that they might keep us in for anything because I didn’t want to risk it. So, as a parent or Carer, it’s important to keep on top of knowing which medications they are on and the dosages Etc., so that you can monitor the actions of others where possible.
What About Side Effects?
Yes, there will be some! One of the side effects of one of the drugs during Phase III was a rash that occurred around my daughter’s mouth which always looked like sores that someone could mistake for an infectious disease. They called it the Mercaptopurine Rash. There was literally nothing we could do at the time to get rid of it. So that was yet another thing that caused social stress due to what other people were, or might be, thinking. It wasn’t a very attractive look and I guess it’s lucky that she was so young and not worrying about going out in public with the rash. I would probably look into doing a detox or some kind of liver support now that I know a little more about the workings of the body with my degree in Health Science. There are supplements and essential oils that might be able to help with this. I knew nothing back then, everything I’ve learned about health has occurred as a result of my desire to know more, help more and understand how my daughter could have become sick in the first place. I should have an article or information booklet that will give some ideas of ways to detox coming soon so keep an eye out for that. I also firmly believe that she developed allergies, which she never had before, as a result of her little body being so overloaded with chemicals, drugs, Etc., that it couldn’t cope anymore.
Conclusion:
In answer to the question of what is the treatment for acute lymphoblastic leukemia in children, this article is an outline of some of what we experienced during my daughter’s own battle with leukemia. Yours may be a totally different story but reading this may give you some pre-warning for what you can expect. It’s important to note that treatment plans are highly individualized, and the specific drugs, dosages, and treatment duration can vary from patient to patient. Healthcare teams closely monitor patients throughout treatment to assess their response and adjust the plan as needed. My secondary article on what you can expect in terms of treatment and the impacts it has (link will be here) will cover other areas of the treatment process because treatment is not only the 3 phases mentioned here, there is more entailed in it.
Take comfort in knowing that ALL treatment has improved significantly over the years, leading to better outcomes for many patients, especially children and young adults. However, the treatment can be intensive and may have side effects, so it’s crucial for patients to work closely with their medical team to manage their care effectively. If you aren’t getting support then you might need to make some waves until you get some help. I didn’t get the help I needed even though i tried and tried for years, people never acknowledged the issues we faced. But now there is much more knowledge on the side effects and after effects so help should be easier for you. Good luck and I hope you will let me know in the comments how your child is doing. Reach out if you would like to connect with others in the same boat.
For now, take care.
Warm Wishes,
Ange


